ASCO 2023 Denver Review: Updates in Metastatic Breast Cancer
Presentation by Dr Anthony Elias, University of Colorado
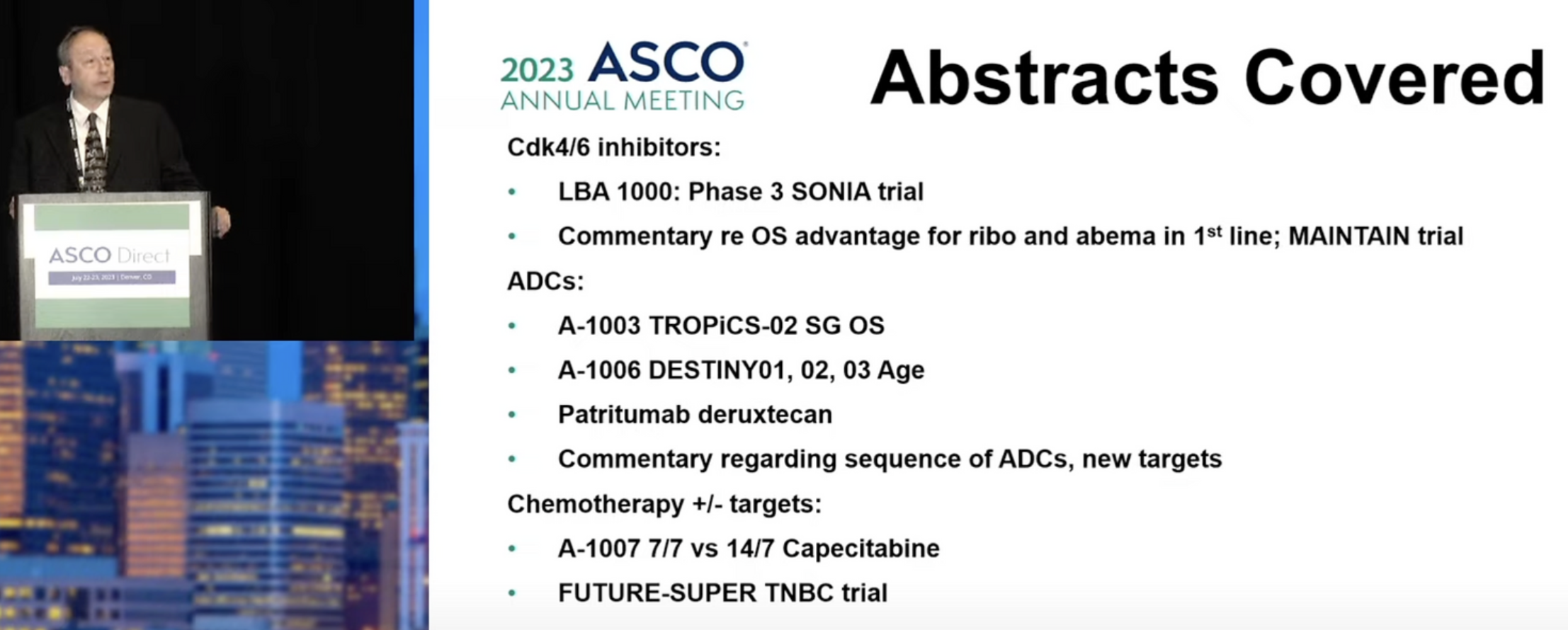
At the Total Health 2023 American Society for Clinical Oncology (ASCO) review held in Denver, Colorado, Dr Anthony Elias, MD, from The University of Colorado presented relevant updates on the topic of metastatic breast cancer (mBC), as reported at the ASCO 2023 Annual Meeting.
CDK4/6 Inhibitors
Dr Elias first reviewed data for the cyclin-dependent kinase 4/6 inhibitor (CDK4/6i) drugs, specifically, results from the Phase III SONIA trial. There are three CDKi currently approved for use in breast cancer (palbociclib, ribociclib, and abemaciclib), and these drugs are used in combination with endocrine therapy (ET), for patients with estrogen receptor positive (ER+) mBC.
In the SONIA trial (BOOG-2017-03), the use of a CDK4/6i in the first line (1L) or second line (2L) setting was compared in a large trial (>1000 patients). The vast majority of patients in the trial (91%) received palbociclib as their CDK4/6i, with the rest receiving one of the two additional CDK4/6i (ribociclib, 8%; abemaciclib, 1%); this is due to the fact that palbociclib was the first of the CDK4/6i to be approved. Patients in SONIA received therapy with a non-steroidal aromatase inhibitor (AI), either with (1L group) or without a CDK4/6i, and this was followed by treatment with a selective estrogen degrader drug, fulvestrant, either with (2L) group or without a CDK4/6i. The primary endpoint of the trial was progression free survival (PFS) after the 2 lines of therapy (termed ‘PFS2’).
The results for the primary endpoint, PFS2, showed no significant difference between the 1L and 2L treatment arms, however, PFS after the first round of therapy (termed ‘PFS1’) did show a significant benefit of using a CDK4/6i in combination with an AI, versus AI therapy alone (median PFS 24.7 vs. 16.1 months), with nearly a doubling of PFS in the first line setting, and Dr Elias noted this was consistent with the primary Phase III findings that resulted in the approval of the CDK4/6i. The result for overall survival (OS) was also not different between the 1L and 2L arms, and the results thus suggest that delaying the use of CDK4/6i is not detrimental. A limitation of the PFS2 findings, Dr Elias noted, is that fulvestrant as a single agent is not considered standard of care in the United States, as it would usually be combined with another agent for such patients. Commenting on the overall findings of the trial, Dr Elias raised the question of whether outcomes might have been different if another CDK4/6i had been used, as palbociclib, unlike the other later approved CDK4/6i, ribociclib and abemaciclib, does not appear to show a survival benefit when used in the first line setting. As such, currently he currently favors the use of CDK4/6i in the 1L setting for ER+/HER2- mBC, with some bias toward using ribociclib or abemaciclib, as these two agents show an OS advantage, albeit with distinct toxicity profiles.
Antibody Drug Conjugates in mBC
Dr Elias then reviewed updates for the antibody drug conjugates (ADCs), a class of drugs that target breast cancer cells using a specific antibody that is fused to a cytotoxic drug (called the ‘payload’). In the TROPiCS-02 trial, the ADC sacituzumab govitecan (SG) was compared to physician’s choice of chemotherapy for patients with hormone receptor positive (HR+), HER2- mBC, and final OS results were presented at this year’s ASCO. Patients in this trial, Dr Elias noted were “heavily pretreated”, having received at least 2, and up to 4 lines of prior chemotherapy for metastatic disease. They also had to have received prior endocrine therapy and a CDK4/6i. Patients (N=543) were randomized to treatment with SG or single agent chemotherapy of physician’s choice (TPC). PFS results out to 18 months continue to show a benefit of SG over TPC (18-month PFS rate 14.4% vs. 4.7%) with a median PFS of 5.5 versus 4.0 months (P<0.0001); the median OS was also significantly better with SG (14.5 vs. 11.2 months; P=0133). In a separate analysis of PFS according to the level of expression of Trop-2, the cell surface target for SG, the results showed a benefit of SG over TPC, even for patients whose tumors had very low Trop-2 expression (median PFS 5.0 vs. 4.0 months, respectively), however the benefit was greater for patients with high Trop-2 expression in their tumors (median PFS 5.8 vs. 4.1 months, respectively).
Dr Elias also reviewed results for another ADC called trastuzumab deruxtecan (T-DXd) which has been used in patients with HER2- mBC, including those who were ER+ and ER negative (ER-), across three different clinical trials (DESTINY-Breast-01, -02, and -03). He described results from a pooled analysis of these trials, which examined the safety of T-DXd according to patient age. The overall findings showed that the occurrence of treatment-emergent Grade 3 or higher adverse events (TEAEs) was roughly similar for the < 65, and > 65 age groups, as well as in the subgroup of > 65 patients who were > 75 years (53.6%, 65.5%, 51.5%, respectively), with a slight trend toward higher TEAEs in the older groups. Similarly, there was a slightly increased risk for interstitial lung disease (ILD)/pneumonitis (one of the rarer but potentially serious side effects of T-DXd) in the older patient group, although Dr Elias noted that the rate of serious ILD/pneumonitis with T-DXd overall has been decreasing as a result of greater clinical experience using the drug. Overall, he noted that T-DXd remains an effective treatment option in the population, with acceptable safety profile in older populations, although additional study of T-DXd in older, frailer, and/or comorbid patients would be useful.
Commenting on the ADCs overall, Dr Elias noted that ADCs are highly active agents in mBC and display lower toxicity as compared with the free agent toxins, and a number of different agents having distinct cellular targets such as HER3 and other agents such as Nectin-4, LIV1 and B7H4 are under investigation in breast cancer. Some drawbacks to the use of these agents he noted include limited data on how to best sequence these agents over the course of treatment (e.g., using SG after T-DXd or vice versa?). Another potential pitfall with ADCs is the limited number of cytotoxic components, or “payloads” used in the drugs; for example ~75% of ADCs utilize an anti-tubulin agent as the payload, ~20% utilize a topoisomerase I inhibitor, and only a small number of ADCs in development utilize alternative toxins. In theory, using one anti-tubulin ADC after another anti-tubulin ADC (with a different target) could result in resistance to all anti-tubulin-based ADCs. A third issue is tumor heterogeneity (meaning differences in antibody target expression across different regions within the same tumor) which could limit the efficacy of these agents and/or lead to resistance.
Chemotherapy
Dr Elias also highlighted the X-7/7 Trial of capecitabine, an orally administered chemotherapy for mBC in his review. This was a small, randomized, Phase II trial that compared the efficacy and safety of capecitabine administered by two different regimens, either the standard (FDA approved) dosing of 1250 mg/m2, twice daily for 14 days with 7 days’ rest (SD), or a fixed dose of 1500 mg/m2, twice daily for 7 days with 7 days’ rest (FD), with the exploratory goal of determining if an equally effective and less toxic dosing regimen for capecitabine could be used. Most of the patients in the trial were ER+/HER2- and had received 1 or fewer lines of prior chemotherapy. The results for PFS (80.8% vs. 83.7%; P=0.98) and OS (median 17.5 vs. 19.8 months; P=0.17) showed no significant difference between the SD and FD regimens. Toxicity, however, was markedly different between the regimens, with significantly less diarrhea (P=0.0008), hand-foot syndrome (P=0.0019), and oral mucositis (P=0.0001) in the FD versus the SD arm. There was also significantly less Grade 3-4 toxicity (27.4% vs. 11.3%; P=0.02), less treatment discontinuation (28.7% vs. 7.5%; P<0.0006), and less dose modification (23.3% vs. 7.5%; P=0.0063) in the FD versus the SD arm. Dr Elias suggested the FD regimen could be an alternative option to minimize toxicity while maintaining good efficacy outcomes, although he did note the small size and the design of the trial, which was not intended to show non-inferiority, nor to provide definitive efficacy data for the regimen. In addition, while the trial results are reassuring, another caveat he noted is that few oncologists are currently using the SD regimen for capecitabine in everyday clinical practice.
2023 ASCO Metastatic Breast Cancer Highlights with Dr Elias:
A Quick Summary
CDK4/6 Inhibitors:
First line use of CDK4/6 inhibitors, in combination with endocrine therapy, is an option for patients with estrogen receptor positive (ER+) mBC, based on findings from the SONIA trial.
Ribociclib or abemaciclib may also offer a survival benefit when used in this setting.
Antibody-Drug Conjugates:
Long-term finding from the TROPiCS-02 trial show that sacituzumab govitecan improves both PFS and OS as compared to physician’s choice of chemotherapy for patients with HR+/HER2- mBC.
Despite a trend toward more adverse events in those > 65, and > 75 years, in a pooled analysis, trastuzumab deruxtecan (T-DXd) showed an acceptable safety profile when used in older populations.
Chemotherapy:
In the X-7/7 Trial, a fixed dose of capecitabine showed comparable efficacy and better tolerability as compared with the standard, FDA-approved dosing regimen.
Dr Elias is Martha Cannon Dean Chair in Breast Cancer Research and Professor of Medicine at the University of Colorado Cancer Center.
Speaker Disclosure Information: Dr Elias reported no disclosures for this presentation.